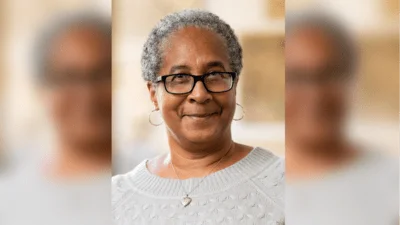
Dr. Manish Khanna | Capitol Breathe Free
Dr. Manish Khanna | Capitol Breathe Free
- Chronic sinusitis affects 28.9 million American adults and is responsible for 4.1 million doctor visits annually.
- Studies show that individuals who suffer from chronic sinusitis experience an increased number of awakenings during a night's sleep.
- It is believed that chronic sinusitis is also a primary contributing factor for snoring and sleep apnea.
"Inflammation of our nasal passages can certainly affect our quality of sleep," Dr. Khanna told the Maryland State Wire. "We know the nose plays a role in snoring and sleep apnea, so when we're dealing with inflamed sinuses, a patient can be prevented from going into deep sleep. So it definitely has a negative impact on sleep when you're talking about acute and chronic sinusitis."
A study published by the National Library of Medicine found that people who suffer from chronic sinusitis are more likely to experience poor-quality sleep. While 8-18% of the general population suffers from sleep disruption, the study found that 60-75% of people with chronic sinusitis experience sleep disruption. The study found that chronic sinusitis patients who experience sleep disruption are also more likely to experience depression, a decreased quality of life, difficulty concentrating, fatigue throughout the day, and decreased memory and productivity.
Signs that your sleep quality could be better include taking more than 30 minutes to fall asleep at night, regularly waking up more than once during the night, experiencing breakouts, having red or puffy eyes or dark circles under the eyes, finding it difficult to concentrate during the day, or feeling tired throughout the day. In addition to chronic health conditions, factors that can contribute to poor sleep quality include stress and anxiety, the absence of a regular sleep schedule, or drinking too much caffeine or alcohol. To improve sleep quality, the Sleep Foundation recommends implementing a consistent sleep schedule, not watching TV or looking at a phone or computer within 30 minutes of going to bed, not drinking alcohol or caffeine before bed, and starting a relaxing bedtime routine. If sleep quality does not improve after implementing those changes, it could be time to consult a doctor.
Many patients who undergo minimally invasive surgery to treat chronic sinusitis find that after the surgery, their quality of sleep drastically improves, according to Atlanta ENT. A study of more than 500 patients who underwent sinus surgery found significant improvement in the patients' sleep quality and overall quality of life.
Sleep Awareness Week celebrates sleep health and encourages the public to prioritize sleep to improve their overall health and well-being. According to the National Sleep Foundation, sleep is a key factor in both physical and mental health. They report that about 65% of Americans who are dissatisfied with their sleep experience worsened health symptoms.
According to Capitol Breathe Free's website, Dr. Khanna earned his undergraduate degree at the University of Maryland, Baltimore County. The following year, he completed his postgraduate research at the National Institutes of Health (NIH). In 2002, he received his medical degree from Albany Medical College. He then secured a place in the otolaryngology residency program at Albany Medical Center, where he completed his surgical internship and residency, holding the position of chief resident until 2007. Following the residency, Dr. Khanna obtained a fellowship in rhinology—advanced endoscopic sinus surgery—at the California Sinus Institute in Palo Alto, California. He concluded his fellowship in rhinology and achieved board certification in otolaryngology—head and neck surgery—in 2008 before returning to the D.C. metro area.





 Alerts Sign-up
Alerts Sign-up